Posted Mar. 30, 2015 at 8:58 AM
Updated Mar 30, 2015 at 8:59 AM
Posted Mar. 30, 2015 at 8:58 AM
Updated Mar 30, 2015 at 8:59 AM
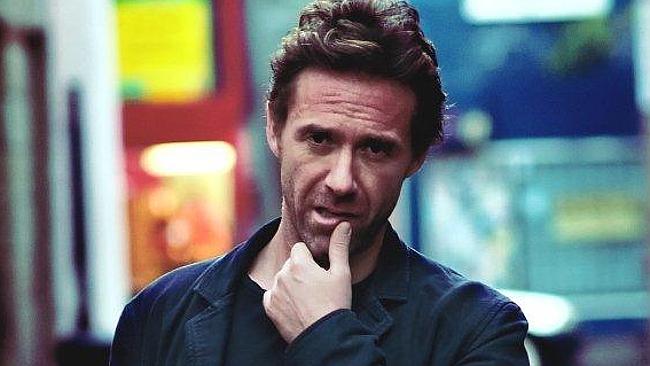
A person with obsessive compulsive disorder often focuses on a partner’s faults rather than the positive aspects of a relationship. Photo: iStock
Q: I am a 42 year-old man with mild obsessive compulsive disorder. I want to settle down and marry, but I can’t fall in love. I haven’t loved any woman since my first girlfriend at 25. I’ve had other relationships (for up to a year) with women I’ve been fond of, and we’ve enjoyed great sex. I feel excited as relationships begin, but then become anxious, disconnected, and then split up. Afterwards, when it’s too late, I feel the love again, but question if it’s real. I come from a loving family, and would love one of my own like my friends, but I can’t imagine feeling strongly enough.
A: OCD (obsessive compulsive disorder) is popularly associated with symptoms such as repeated hand washing, extreme tidiness and a need for order or symmetry, or as an irrational fear of germs. This syndrome can also manifest as a problem in maintaining relationships (both romantic and social).
Intimate relationships are important for a person’s wellbeing, so they can easily become an area for obsessions. Some people with relationship OCD have obsessions about how they feel in a relationship, or how they felt in past relationships.
It is normal to experience doubts and anxieties as a relationship develops. However, in ROCD, such preoccupations are chronic and intrusive, unwelcome but unstoppable, and quite disabling, affecting the sufferer’s ability to fall in love.
Fear of making a mistake can cause a person with ROCD to keep asking for reassurance, to continuously doubt whether they love their partner, whether their relationship is the right one, or to doubt that their lover really loves them.
When people with ROCD are pretty sure they are in a loving relationship, they might still constantly check and reassure themselves that it is the right feeling. They often nit-pick and find fault. Instead of finding good in their partner, they focus on shortcomings, often exaggerating them and using them to prove the relationship is bad.
This inability to concentrate on anything but a partner’s flaws causes great anxiety, and strains the relationship. However, when they attempt to end a relationship, they are then overwhelmed with anxiety about whether that was a mistake, and maybe she was actually “the one” and they have blown it. Nothing ever just feels comfortable and right.
Psychological and biological factors are thought to play a role in the development and maintenance of all forms of OCD. When a person relies too heavily on his or her intimate relationships for feelings of self-worth, or where someone has a fear of abandonment, this can contribute to ROCD.
You mention the failed romance of your youth, saying that woman was the only one you have ever loved. Was the ending of that relationship distressing and traumatic? Did your fear of getting it wrong play a negative role at that time? What was it about her that you loved, and that all other women lack? I suspect some of the clues to your current distress will be found in that relationship.
It is a truism that you cannot love someone else before you love yourself. When you are complete in yourself, you do not look for a partner to complete you. You see the other person as an individual, live in the moment, and make calm, measured assessments about how it’s going. You do not approach your lover in a needy way, cling to them for fear of rejection, or criticise them in case you make a mistake and get trapped.
In order to break out of a cycle of behaviour that is not serving you, you need to change the wording of the thoughts that revolve in your mind. Cognitive behavioural therapy is very effective in helping you to do this. So is exploring the concept and practice of mindfulness.
For more information about ROCD, and to find resources that might be useful, take a look at websites such as rocd.net.
If you feel you could do with some professional help with your struggle, consider seeing a psychologist or relationship therapist who has experience with treating suffers of OCD.
Email your questions to abtlastnight@gmail.com.
At 13 years old, I was afraid to touch floors, door knobs, bus seats or even walk into a room without feeling contaminated and having to compulsively wash my hands until I felt the fear had rinsed off. Anxiety has always been a major part of my existence, and although it’s not something I take pride in announcing, it usually speaks for itself. “You need to relax; just don’t think about it,” would be easier to hear if it were that easy. But neurochemically, I can’t. From the obsessive counting, worrying, muscle tics, the double, triple and then quadruple checking, anyone with an anxiety disorder can promise you: We honestly can’t just “calm down.”

According to the Anxiety and Depression Association of America, anxiety disorders are the most common mental illness in the United States, affecting nearly 40 million adults in the United States age 18 and older, which is about 18 percent of the population. Obsessive compulsive disorder (OCD), a type of anxiety disorder that is also considered its own condition, occurs in about 2.2 million in the U.S., equating to about 1 percent of the population. On the most basic neurological level, the amygdala, a brain structure associated with triggering our fear reactions, plays a central role in anxiety disorders. Those who tend to be more anxious have been observed to have larger than average amygdalae.
For people with anxiety disorders, the anxiety manifests as an itch we need to scratch, and maybe if we scratch it, it’ll go away. The problem is that it never does. For OCD, there are quirks, but then there are compulsions. Sometimes I won’t realize I’m ripping my hair unless someone who’s been watching me do it for the past 20 minutes points it out.
Typically, when others hear about obsessions they think about lining up colored pencils and not the reality of “If I don’t close this door seven times then my dog will die” ranging to “I’m afraid that I’m going to accidentally kill my dog.” It’s desperately seeking control of your own life by letting your anxiety control it for you.
The “anxiety” buzzword has been diluted down to a catchphrase. The moment I bring up my excessive worrying everyone else has already ordered a season pass to join the OCD club because, hey, everyone has anxiety, right? Empty reminders to just “chill out” and “stop worrying so much” are tossed around as passive-aggressive punchlines because others fail to realize my anxiety doesn’t take vacations.
Telling someone “It’s all in your head” is only stating the obvious. Of course it’s in my head; where else would it be? I’m fully aware that checking, and re-checking, and re-checking and … checking again to see if my coffee cup is across the room from my laptop because if not my room will set fire isn’t rational thinking, but there’s no use in reminding me that. No one who performs ritualistic compulsions will be miraculously cured when you remind them of how silly it is. The problem is that we already know.
I don’t expect others to put up with what I have to, and that’s why I understand that when I have to repeat “I’m sorry” 11 times until it sounds right, most people stop listening. “Calm down” is simply an empty phrase that comes from mouths that don’t speak the language of anxiety. I’ll never know how it feels to live without generalized anxiety, but I can live without the constant reminders from others about how to deal with it.
The treatment of prisoners with mental illness is often barbaric if not medieval. Here’s what needs to stop.
At some point in the 1970s the decision was made to close state-run mental health institutions. Much of this was motivated by The Community Mental Health Act in 1963. Reports at the time indicated significant abuse of patients and a general lack of credible mental health care. The idea was that funds would be redirected from the states to local communities to manage and monitor the needs of individuals with mental health issues. Unfortunately, this transfer of funds never happened and local communities were simply overwhelmed.
The result was that many people with mental illnesses found themselves in the prison system. Systems underfunded and understaffed without training who were primarily focused on incarceration rather than the needs of anyone with a health condition defined by mental illness.
To make matters worse, prisoners suffering from mental illness often found their condition exacerbated and amplified by their incarceration. Imagine a person suffering from depression or bipolar disorder in a hostile and restrictive environment. The new solution in fact created significant problems and ignored a landmark ruling from the Supreme Court.
What has essentially happened is the trans-institutionalization of mental illness from hospitals to prisons. And the prisoners with mental health conditions suffer greatly. Some become withdrawn and others find themselves in solitary confinement intended as a protective measure. According to a report submitted by the University of Pennsylvania in February, 2011: “Incarceration has a robust relationship with subsequent mood disorders, related to feeling ‘down,’ including major depressive disorder, bipolar disorder, and dysthymia.”
The fact of the matter is that anyone in solitary confinement is treated the same way. They are ignored and only allowed one hour a day to walk into a walled or caged area. They are given their meals in their cell, and windows are small and rare. Solitary is often used as a punishment room, but in many prisons it’s used as way to keep mentally ill prisoners away from the general prison population while imposing the worst punishment a manic-depressive or schizophrenic person could endure.
To make matters worse, many people incarcerated are not properly diagnosed before sentencing. If someone appears to have a substance abuse issue, they are assumed to tolerate withdrawal from that addiction cold turkey when denied access to substances in prison. Most tough it out. Unfortunately, undiagnosed individuals with serious mental disorders like schizophrenia or bipolar disorders are often sent into prisons without proper diagnosis or any plan for treatment or medications. The result is their condition worsens.
Based on a range of studies done by the National Institute of Mental Health, The American Journal of Psychiatry, the U.S. Department of Education and other sources:
- One in four adults -− approximately 61.5 million Americans -− experiences mental illness in a given year. One in 17 -− about 13.6 million -− live with a serious mental illness such as schizophrenia, major depression or bipolar disorder.
- Approximately 20 percent of youth ages 13 to 18 experience severe mental disorders in a given year. For ages 8 to 15, the estimate is 13 percent.
- Approximately 1.1 percent of American adults — about 2.4 million people — live with schizophrenia.
- Approximately 2.6 percent of American adults -− 1 million people -− live with bipolar disorder.
- Approximately 6.7 percent of American adults -− about 14.8 million people -− live with major depression.
- Approximately 18.1 percent of American adults -− about 42 million people — live with anxiety disorders, such as panic disorder, obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), generalized anxiety disorder and phobias.
- About 9.2 million adults have co-occurring mental health and addiction disorders.
- Approximately 26 percent of homeless adults staying in shelters live with serious mental illness and an estimated 46 percent live with severe mental illness and/or substance use disorders.
The fact of the matter is that our prisons are populated by people in desperate need of caring and sensitive psychiatric care. Unfortunately the opposite is true. Both police officers and prison guards receive very little training with regards to interactions and managing individuals with mental illness. Programs need to be initiated to increase that awareness and sensitivity, and most importantly — how to approach and manage someone who has a severe mental illness.
Currently, the prison solution is the worst. Solitary confinement continues to be the method of choice in U.S. prisons for anyone demonstrating perceived or misunderstood mental illness. It is perhaps the most severe and cruel form of punishment for anyone suffering from a severe mental illness. The result is that many people who enter prison with a mental illness leave prison with a condition that is worse. “The lack of treatment for seriously ill inmates is inhumane and should not be allowed in a civilized society,” Dr. E. Fuller Torrey, founder of the Treatment Advocacy Center, said in a recent report.
The result is that many people with mental illness who are incarcerated find themselves back in prison again. The fact of the matter is that our mental health system has failed as the federal government continues to deny and ignore the promises made to improve the system by taking responsibility from the states.
The result is that recidivism rates among the mentally ill is soaring. Any hopes of rehabilitation based on any criminal activity are outweighed by the intense and long-lasting affects of incarceration on mentally ill individuals.
It seems obvious that the best recourse is to return responsibility for the management of mental illness to the states. This appears on the surface to be problematic given the fiscal distress so many states are enduring, but with adequate federal funding the solution is workable. There is also a need for both federal and state funds to be allocated to communities.
On a fundamental level we must overcome our fundamental fear and intolerance of mental illness. We all know someone among our family and friends who struggles with an addiction or a mental disorder and we need to extend that same compassion and care we feel towards them to others.
As potential employers we should not stigmatize people with a police or prison record. Without the potential for employment they will forced to a vicious cycle of hopelessness and potentially crime.
Most importantly, we need to do something about the failure of our prisons as a repository for the mentally ill. Through a series of unintended consequences we’ve sabotaged our mental health system and relegated the management of mental illness to a penal system designed to imprison and punish.
In a controversial statement made on March 10, 2011, Martin Harty, a member of the New Hampshire state legislature, was asked what could be done for the state’s mentally ill homeless people. Harty replied that the state should “Rent a spot in Siberia for them.” The media was indignant but ironically, mentally ill homeless persons now receive better care in most parts of Siberia than they do in most parts of New Hampshire.
Save. Preview. Save. Preview. Save. Preview. No, these are not different posts waiting to be published online, they are the same post being obsessively checked by me, a sufferer of Obsessive Compulsive Disorder (OCD). It’s not something that hits me every time I finish a piece of writing but it does quite often.
If you have any knowledge of OCD and aren’t a sufferer yourself, the chances are quite high that you think of it as that hand-washing door-lock checking thing that looks weird but seems largely harmless. The truth of the matter is that OCD can attach itself to anything that is important to the sufferer and so can be far more varied or obscure than the commonly held beliefs above. It can also change form over the years, even if the themes stay the same. How about a sufferer obsessed with germs and hand-washing suddenly finding themselves obsessively scanning their PC for viruses every day? Or the gadget geek who is so afraid that something might be wrong with a newly purchased toy that they examine it with the concentration usually utilised by forensics at a crime scene? Technology has changed the world around us, so is it any wonder that our mental issues have reached the next version number too? If you have OCD and happen to be a geek, it will almost certainly poke its nose into your favourite hobbies and interests.
OCD is an anxiety disorder that causes the sufferer to feel tremendous amounts of anxiety about certain things which are triggering issues for them. The sufferer feels the overwhelming urge to engage in certain behaviours to lessen these uncomfortable feelings, be it checking that the door really is locked or engaging in mental checking or patterns of thought. Geeky pursuits can often be a great way to offset some of the effects that this disorder has on a person, either by engaging the brain, mentally escaping to somewhere otherworldly, or simply used as a common basis for social interaction. Until OCD begins to come along for the ride that is.
I used to play the MMORPG World of Warcraft. I hadn’t been on it for too long when I decided to create a new character; I very much wanted to try playing as a sneaky Rogue rather than the cloth-wearing Mage class. I played for a while and then began to feel anxious about whether I’d made the right character choice. Fast forward a week or so, and I’d made and discarded almost ten new characters, never settling with one or feeling ‘right’, my anxiety levels going through the roof every time I sat at the login screen. What had been an enjoyable pastime had become one more thing for my OCD to beat me with. I did get past it, but I felt both foolish and weak afterwards. The anxiety I felt was tremendous. This wasn’t just “My CD’s aren’t organised and it bothers me!” levels of anxiety, this was almost at panic-attack levels. Creating a new character in an online game sounds like such a trivial thing, but when OCD begins to twist it into something more important, it becomes as trying as fears of germs and unlocked doors.
OCD makes the sufferer hyper-vigilant for incoming catastrophes or any signs of possible problems in the future, but sadly for the sufferer, almost everything feels like one. That new home cinema system you bought with the little fan spinning at the back…should it be that noisy? Your laptop usually boots in a few seconds, why did the last boot take what seemed like a minute? That USB cable didn’t feel right as you plugged it in did it? What if the port is faulty? What if there is a problem that makes it unsafe and it sparks and starts a fire? To a non-sufferer, this sounds like a low-budget Final Destination scenario playing out. A sufferer will have all kinds of fears and associations like this clicking into place every time their anxiety surges. It’s a perverse kind of creativity, one that enslaves you rather than frees you. I’ve turned the tables on mine and chained it to my writing desk. I poke it with a sharp stick and it helps me with my horror fiction; a just reward for making my own life hell at times.
Thankfully, OCD is treatable. My own path to a better understanding came through Cognitive Behavioural Therapy and self-eduction via some very good books on the topic. If you think you might have OCD, consult your Doctor, as this is one illness that does have treatments available that can help you come to terms with it and begin to deal with it in a more skilful way.
First posted on Geek Syndicate.
Save. Preview. Save. Preview. Save. Preview. No, these are not different posts waiting to be published online, they are the same post being obsessively checked by me, a sufferer of Obsessive Compulsive Disorder (OCD). It’s not something that hits me every time I finish a piece of writing but it does quite often.
If you have any knowledge of OCD and aren’t a sufferer yourself, the chances are quite high that you think of it as that hand-washing door-lock checking thing that looks weird but seems largely harmless. The truth of the matter is that OCD can attach itself to anything that is important to the sufferer and so can be far more varied or obscure than the commonly held beliefs above. It can also change form over the years, even if the themes stay the same. How about a sufferer obsessed with germs and hand-washing suddenly finding themselves obsessively scanning their PC for viruses every day? Or the gadget geek who is so afraid that something might be wrong with a newly purchased toy that they examine it with the concentration usually utilised by forensics at a crime scene? Technology has changed the world around us, so is it any wonder that our mental issues have reached the next version number too? If you have OCD and happen to be a geek, it will almost certainly poke its nose into your favourite hobbies and interests.
OCD is an anxiety disorder that causes the sufferer to feel tremendous amounts of anxiety about certain things which are triggering issues for them. The sufferer feels the overwhelming urge to engage in certain behaviours to lessen these uncomfortable feelings, be it checking that the door really is locked or engaging in mental checking or patterns of thought. Geeky pursuits can often be a great way to offset some of the effects that this disorder has on a person, either by engaging the brain, mentally escaping to somewhere otherworldly, or simply used as a common basis for social interaction. Until OCD begins to come along for the ride that is.
I used to play the MMORPG World of Warcraft. I hadn’t been on it for too long when I decided to create a new character; I very much wanted to try playing as a sneaky Rogue rather than the cloth-wearing Mage class. I played for a while and then began to feel anxious about whether I’d made the right character choice. Fast forward a week or so, and I’d made and discarded almost ten new characters, never settling with one or feeling ‘right’, my anxiety levels going through the roof every time I sat at the login screen. What had been an enjoyable pastime had become one more thing for my OCD to beat me with. I did get past it, but I felt both foolish and weak afterwards. The anxiety I felt was tremendous. This wasn’t just “My CD’s aren’t organised and it bothers me!” levels of anxiety, this was almost at panic-attack levels. Creating a new character in an online game sounds like such a trivial thing, but when OCD begins to twist it into something more important, it becomes as trying as fears of germs and unlocked doors.
OCD makes the sufferer hyper-vigilant for incoming catastrophes or any signs of possible problems in the future, but sadly for the sufferer, almost everything feels like one. That new home cinema system you bought with the little fan spinning at the back…should it be that noisy? Your laptop usually boots in a few seconds, why did the last boot take what seemed like a minute? That USB cable didn’t feel right as you plugged it in did it? What if the port is faulty? What if there is a problem that makes it unsafe and it sparks and starts a fire? To a non-sufferer, this sounds like a low-budget Final Destination scenario playing out. A sufferer will have all kinds of fears and associations like this clicking into place every time their anxiety surges. It’s a perverse kind of creativity, one that enslaves you rather than frees you. I’ve turned the tables on mine and chained it to my writing desk. I poke it with a sharp stick and it helps me with my horror fiction; a just reward for making my own life hell at times.
Thankfully, OCD is treatable. My own path to a better understanding came through Cognitive Behavioural Therapy and self-eduction via some very good books on the topic. If you think you might have OCD, consult your Doctor, as this is one illness that does have treatments available that can help you come to terms with it and begin to deal with it in a more skilful way.
First posted on Geek Syndicate.
Jesse Fink, author of The Youngs, The Brothers Who Built AC/DC Picture: Supplied
Source: Supplied
Poet Neil Hilborn tells the emotional story of falling in love with a girl as a teenager while he struggled with severe obsessive compulsive disorder. Courtesy Button Poetry
MANY men don’t know what to do in moments of crisis or when dealing with mental illness. I know this from personal experience. From about the age of 30, I was one of these men. I had no idea where to turn or who to turn to. I seriously contemplated suicide a number of times. After a catastrophic divorce, my life was rapidly spiralling out of control.
I’m still here. I’m the author of three books and one e-book, I am father to a wonderful 11-year-old girl, and have a good professional and personal life. I’m healthier at 41 than I was at 21, but when I look back on my 30s, I see a decade lost. I lost it mostly to obsessive-compulsive disorder or OCD, an anxiety-spectrum disorder that affects hundreds of thousands of Australian men, women and children, of whom very few will ever talk about it openly. It’s very much a debilitating hidden illness.
It’s also one of the most misunderstood disorders and part of the motivation in a lot of my work — my writing and my public speaking — is to help people who are dealing with depression, OCD and other anxiety disorders every day of their lives. You’re not on your own and never will be. There are people out there who understand what you’re going through and help is there if you need it.
It’s no fun to live with OCD. People who have it deal with it by trying to maintain a front that everything is fine and they’re OK. They’re not. They’re really suffering.
I can’t tell you the number of times I’ve wanted to scream when some celebrity who is fastidious about cleaning their fridge or sorting their shoes has said they’re “so OCD”. It’s almost an insult to someone who’s really going through the worst of what this disorder involves.
OCD is a very serious condition, not simply an amplified need for cleanliness or order, such as David Beckham’s obsession with pairs or Jessica Alba’s fastidious hair-brushing, which is actually OCPD (obsessive-compulsive personality disorder).

Handwashing is a familiar symptom of OCD. Photography: David Kapernick
Source: News Limited
The rituals we’re all reasonably familiar with as symptoms of OCD — the counting, the handwashing, the hoarding, the checking, etc. — are all compulsive rituals designed to neutralise the things outsiders can’t see: the intrusive thoughts, images, words and impulses afflicting people with OCD. And when I say thoughts, images, words and impulses, I mean the worst of the worst. A general rule of thumb with understanding the O in OCD is that whatever is the worst thing you can think of, you will think it. So: vivid images of violent acts, abhorrent sexual thoughts. Sudden urges that make you feel as if you want to do something you really don’t want to do.
It’s like living in your own personal 24-hour-a-day horror movie.
So you can appreciate why very few people will admit to having OCD.
That’s because they fear what people will think of them if they confess to having these obsessions, let alone talking about the content of them. These intrusive thoughts, images, words and impulses are especially stressful and upsetting to the sufferer.
The rituals we’re all reasonably familiar with as symptoms of OCD — the counting, the handwashing, the hoarding, the checking, etc.
Source: Supplied
OCD feeds off what is most important to you: the people you love and care about. Or it latches onto the things you subconsciously fear or find most repulsive and uses those worries to invoke scenarios in your mind, completely involuntary on your part, that are the most disturbing and inappropriate of all.
The more you try to avoid thinking something, the more the intrusive thoughts, images, words, urges and impulses (harm obsessions, sexual obsessions) arrive in your mind. Relationships — romantic and family — are a minefield. It’s very typical for an OCD sufferer to just prefer to be alone. They don’t want to be thinking horrible things about the people they love. Who would? So they retreat from their families and friends. They become reclusive. They refrain from sexual intercourse.
People with OCD are capable of rational thought as much as anyone else. This is the great contradiction of the disorder.
But here’s the rub. The rational mind understands that these thoughts, images, words and impulses are not expressions of one’s true self and one’s true desires, but always there is this lingering doubt that maybe you’re wrong; that you’re kidding yourself. Which is why OCD is sometimes called the ‘doubter’s disease’.

The horror of OCD can invade every corner of a sufferer’s life. Photography: Thinkstock.
Source: Supplied
So it never really goes away and this never-ending, relentless cycle of obsession and compulsion takes hold of you and can very nearly ruin your life. And it very nearly ruined mine.
That was until I got a hold of it, changed some habits and approached managing OCD in a methodical and complete way, involving different strategies. I have eliminated symptoms of OCD from my life because I made my recovery my full-time project. I bit the bullet and got help. I talked to people. Organisations such as the Black Dog Institute in Sydney, my friends and doctors gave me the support I didn’t think I was going to get but desperately needed.
The person I am today is very different from the one I was when OCD entered my life. Not just mentally and emotionally but physically. I’ve lost 35kg since 2007, the year when I divorced. For a long time, I couldn’t see my genitals when I looked down. I had a double chin. I dressed like a fat Russell Crowe: all baseball caps and big men’s polo shirts from Kmart.
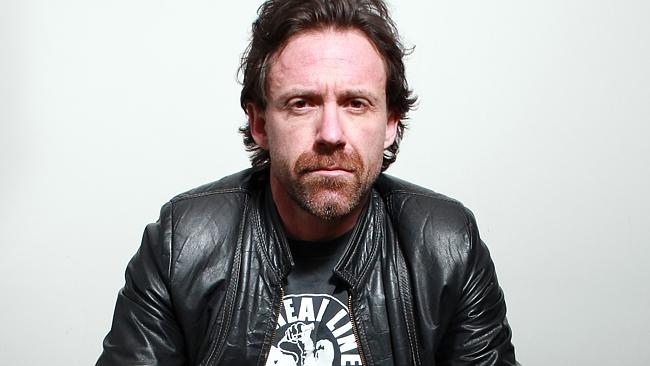
Pictured Author Jesse Fink at the Citigate Hotel in Sydney.
Source: News Limited
I lost all that weight the hard way. There were no tricks. Just discipline and diet. It was exhausting but I persevered. And the best thing was that the more I worked on my physical health, the more my mental and emotional health improved. Simple perseverance and commitment to fitness in turn improved the way my head was working. It is my personal belief that not nearly enough emphasis is put on physical health in the national debate about mental illness.
I’ve found it’s helped me immeasurably to be open about my experience, rather than hiding from people and pretending that part of my life never happened. Half a dozen close personal male friends have since come to me and admitted they’ve been dealing with depression or anxiety for years but felt like they couldn’t talk to anyone. Others are going through the excruciating pain of divorce or relationship breakdowns. It’s happening around Australia every day.
Beyond Blue is the national depression and anxiety initiative. Visit beyondblue.org.au.
Follow Sunday Style on Twitter @sunday_style
Posted Mar. 19, 2015 at 9:59 PM
Updated at 7:59 AM
Joyable is launching today with a simple goal: curing people of anxiety and depression. So Joyable is debuting its web service people can use to track and eventually improve their mental condition. Joyable has also assembled a group of coaches who can motivate participants and keep them engaged with the app.
The startup is also announcing today that it’s raised $2.05 million in seed funding. The new backing comes after the venture-powered rise of startups like Lumosity and Memorado, which have pushed apps people can use to train their brains. The model calls to mind massively open online courses from startups like Coursera and Udemy, except that coaches can help you actually finish what you start with Joyable.
Joyable’s system revolves around a process called cognitive behavioral therapy.
“It is very well established in terms of its clinical opportunity,” Joyable cofounder and chief operating officer Steve Marks told VentureBeat in an interview. “It works equally well without a therapist if you do the exercises. It works in self-help format.”
Rather than requiring people to visit their therapists for a long sitting, then, Joyable is allowing people to go through their therapy in very small doses, from anywhere, so long as you have an Internet-connected computer or mobile device handy.
The therapy lasts for 12 weeks on average. It costs $99 a month, and people can pay $239 for a three-month package. More than 50 people have participated in a pilot. Marks didn’t want to say how many people are currently customers, but he said the number keeps doubling month over month.
Eight people work for San Francisco-based Joyable. which started in 2013. Thrive Capital and Harrison Metal led the seed round. Angel investors like Andy Rachleff also participated.
Going forward, Marks and fellow cofounder Peter Shalek want to expand Joyable’s reach. In the future, the startup could introduce web-based treatments for obsessive compulsive disorder, post-traumatic stress disorder, and depression.
Powered by VBProfiles

THERE are more web-connected devices than people in the world. Smartphones, fitness armbands, cars, factories and even domestic appliances churn out a constant stream of live data. Cheap sensors and the tsunami of information they generate can improve our lives; black boxes in cars can tell us how to drive more carefully and wearable devices (like the forthcoming Apple Watch) will nudge us toward healthier lifestyles. Yet while consumers and surgeons general may welcome such developments, they pose an existential threat to some insurers. How might data-gathering devices spell doom for parts of the insurance business?
Insurance relies on a dynamic of imperfect information. Individuals are at greater or lesser risk of all sorts of ills, from car accidents to cancer. But because those at lowest personal risk of trouble are not always aware of their good fortune, they seek insurance against trouble alongside those with greater propensities to fall seriously ill or face other hardships. Unlucky and lucky alike pool premiums into a collective fund, and the unused payments of the fortunate cover the costs of the unfortunate, leaving some money left over as insurer profits. But the uncertainty that underpins the need for insurance is now shrinking thanks to better insights into individual risks. The growing mountain of personal data available to individuals and, crucially, to firms is giving those with the necessary processing power the ability to distinguish between low-risk and high-risk individuals (and those in between). Thanks to technological innovation, sensors that monitor our every move are becoming cheaper, cleverer and more ubiquitous.

This could upend existing insurance business models, in a few ways. The better behaviour resulting from smart devices is one threat. Conventional risk pools (for home or car insurance, for example) are shrinking as preventable accidents decline, leaving the slow-footed giants of the industry at risk. Business is instead moving to digital-native insurers, many of which are offering low premiums to those willing to collect and share their data. Yet the biggest winners could be tech companies rather than the firms that now dominate the industry. Insurance is increasingly reliant on the use of technology to change behaviour; firms act as helicopter parents to policyholders, warning of impending harm—slow down; reduce your sugar intake; call the plumber—the better to reduce unnecessary payouts. Yet this sort of “Big Mother” relationship relies on trust, and the Googles and Apples of the world, on which consumers rely day-by-day and hour-by-hour, may be best placed to win this business. Most tech giants are now rushing to build health platforms. It doesn’t take a leap of imagination to envisage this approach extending to monitoring of homes, automobiles, and much else besides.
Whether technology companies are actually keen to get into the insurance business is not yet clear. The prize for the most successful firms will probably be huge; last year insurers collected an estimated $338 billion in profits. But the industry will also face intense regulatory scrutiny, as governments seek to make sure that the misfortunes of bad genes or bad luck do not leave some individuals uninsurable and bankrupt. And as the financial crisis reminded us, good but limited data and powerful algorithms still leave plenty of room for the disastrous accumulation of risk. There are some dangers against which even the Apple Watch cannot protect us.
Dig deeper:
Insurers are becoming behavioural engineers (March 2015)
Separating bad behaviour from bad genes is no easy feat (March 2015)
PEMBROKE — Oct. 19, 2014, is a day Melissa Locklear Foust will never forget. It’s the day her “social butterfly” of a daughter, 5-year-old Jazlyn, practically became a different child.
“Lord, I remember it like it was yesterday. We get to [Pembroke Elementary School] and she just totally goes into an anxiety attack like I have never seen. She’s screaming, she’s kicking, she’s fighting and I was in total disbelief,” Foust said.
Jazlyn had been having migraines, which no one else in the family gets, and Foust thought the episode may have been caused by medications prescribed to treat the debilitating headaches. But it happened again the next day.
A local psychologist labelled it anxiety, but Foust felt there had to be more to this sudden change.
“I knew something was wrong but I didn’t know what was wrong,” Foust said.
That’s when a doctor told her about PANDAS.
Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections is characterized by a sudden onset of symptoms associated with Obsessive Compulsive Disorder, Tourette’s Syndrome and other tics after a child has had strep throat.
The disorder is somewhat controversial — studies haven’t shown the causal relationship between the infection and OCD-like symptoms that may arise later. Not much is known about PANDAS’ long-term effects, why the disorder arises, or even how many children have it.
“… The problem is that strep is so common, how do you know it’s not just a kid with OCD, or that something neurologically has changed?” said Dr. Fasil Mohomed, pediatric hospitalist with Southeastern Regional Medical Center and Lumberton Children’s Clinic.
Some researchers believe that a misguided immune response to the infection interferes with the part of the brain associated with learning, voluntary movements and in general choosing what behaviors to employ.
It can be tricky to demonstrate that a child has PANDAS. It’s newly described and there’s no simple test to prove a child has it. The diagnosis process is further complicated by the fact that the disorder typically develops in children ages 4 to 9, when they may be forming new behaviors and are becoming increasingly able to express their ailments.
But parents of children with PANDAS and closely related disorders say the changes they’ve seen in their children’s personalities and mannerisms are all too real. The tics, mood swings and loss of appetite may gradually improve, but parents like Foust say they reappear in full force when the child is again exposed to an infection, like strep.
Before she got sick, Jazlyn was an active child — she danced, she played soccer, she loved to wear girly clothes.
Now, when her symptoms are bad, she has little appetite and as a result has lost weight. At least once she became afraid that if she ate she would choke. She has fits of rage over the mention of going to school, washes her hands repeatedly and blinks so often she has tried to hold her eyes open with her index finger and thumb. Foust said “in our PANDAS world” this is called a flare-up — and other parents of children with the disorder say they experience the same thing.
“She may be in a complete flare up for a whole hour … but she doesn’t remember what she does,” Foust said.
Doctors at Duke recently adjusted Jazlyn’s diagnosis to PITANDS, or pediatric infection-triggered autoimmune neuropsychiatric disorders, which is closely related to PANDAS but can result from any infection. Blood tests have shown Jazlyn has had strep.
Children with the disorders are sometimes put on antibiotics to help them fend off infections, and may benefit from the same therapy children with anxiety disorders would get. Jazlyn has been on and off of antibiotics recently, and Foust says she’ll stay on them, at least until an appointment with Duke University doctors later this month. There, she’s hoping doctors will flag Jazlyn as a candidate for IVIG, a blood product that is administered intravenously and has been shown to help many autoimmune illnesses.
“We’re about ready to try anything that will work so we can get our life back and she can be a regular 5-year-old,” Foust said.
Coming in contact with just about anyone sick has worsened Jazlyn’s symptoms, Foust said — even a stomach virus has sent her down the PANDAS/PITANDS roller coaster. Because of the risk of exposure and Jazlyn’s new habits, she can’t attend school and won’t at least for the rest of what would have been her kindergarten year.
Foust says she has been told her child is the only one in the Public Schools of Robeson County with the disorder, although her cousin’s 3-year-old daughter has begun developing symptoms. On one hand, she believes that could be correct — although grade students can get strep throat infections as many as three times a year, PANDAS is rare.
On the other hand, she wonders how many parents and doctors have not connected the dots when a child gets an infection and sometimes months later develops seemingly unrelated tics. Depending on who you ask, PANDAS and PITANDS are either under-diagnosed because of a lack of awareness about the disorders, or over-diagnosed as distraught parents search for an explanation of what has happened to their child.
Mohomed recommends that parents who believe their child may have PANDAS or PITANDS consult a doctor, and consider visiting a therapist or behavioral specialist.
For her child and for others who may unknowingly have PANDAS or PITANDS, Foust wants to spread awareness of the disorders in Robeson County. She has helped start a PANDAS awareness and support group, which will hold its first meeting April 18 at 10 a.m. at the Robeson County Health Department. Foust encourages parents to have blood tests done when they think their child may have strep as throat cultures sometimes come back negative despite an infection.
“If you know something is different about your child, don’t stop. People are going to tell you “oh, it’s just them being a kid, it’s not strep … This is totally real. My daughter is living proof.”
Sarah Willets can be reached at 910-816-1974 or on Twitter @Sarah_Willets.
A UA professor researching treatment methods for obsessive-compulsive disorder using smartphone apps will be giving a talk on the anxiety disorder today. Cary Jordan, an expert in the treatment of OCD and a UA professor at the College of Education, will be speaking at the college at 5:30 p.m. in Room 318 specifically about pediatric obsessive-compulsive disorder.
Jordan has successfully treated OCD in adults and children and said the response rate has been 85 percent or above for the patients he has treated.
Michelle Perfect, an associate professor and interim program director of the psychology program, said “nearly 20 percent of school age students experience significant social, emotional or behavior difficulties that impact their ability to learn.”
Jordan has been treating OCD since 2007 and said the goal of the pediatric OCD lecture is to “build awareness in the community with regards to what is OCD and what is the evidence-based effective treatment.”
Courtesy of Laura Jordan
Cary Jordan, a professor at the College of Education, will be holding a lecture on pediatric obsessive-compulsive disorder. The talk will be about research he has been performing about the anxiety disorder and the lives of those living with it.
Perfect’s research is focused on the relationship between physical and mental health, and particularly the impact of sleep and other chronic illnesses on mental health and education.
“Despite the high prevalence, up to 80 percent of youth do not receive services,” Perfect said.
Perfect added that the lecture is meant to provide trainees and practitioners with knowledge about cutting-edge research-based treatment for OCD.
“I think the overuse of OCD has maybe drawn attention away from what it is really like to have OCD and how impairing this disorder can be for those diagnosed,” Jordan said.
Jordan said the symptoms of OCD have different degrees of severity and, if left untreated, can consume an individual’s entire life.
“Even moderate levels of symptom impairment can be very impairing,” Jordan said.
_______________
Follow Terrie Brianna on Twitter.
Much like the majority of the season for the No. 5 overall and No. 1 seed in the Pac-12 tournament Arizona Wildcats, things were dicey before the team pulled away later in the action.